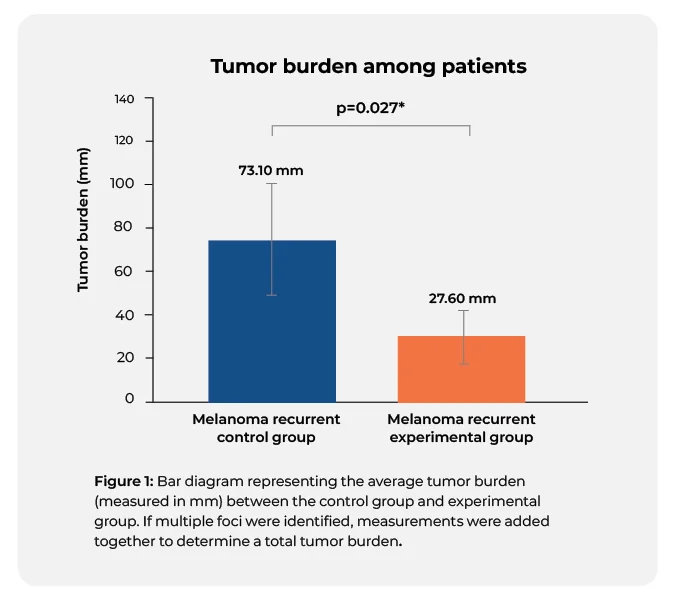
Routine imaging guided by a 31‑gene expression profile assay results in earlier detection of melanoma with decreased metastatic tumor burden compared to patients without surveillance imaging studies
Dhillon S, Duarte-Bateman D, Fowler G, et al. Routine imaging guided by a 31‑gene expression profile assay results in earlier detection of melanoma with decreased metastatic tumor burden compared to patients without surveillance imaging studies. Archives of Dermatological Research. 2023. https://doi.org/10.1007/s00403-023-02613-6
Want to learn more about
DecisionDx-Melanoma?