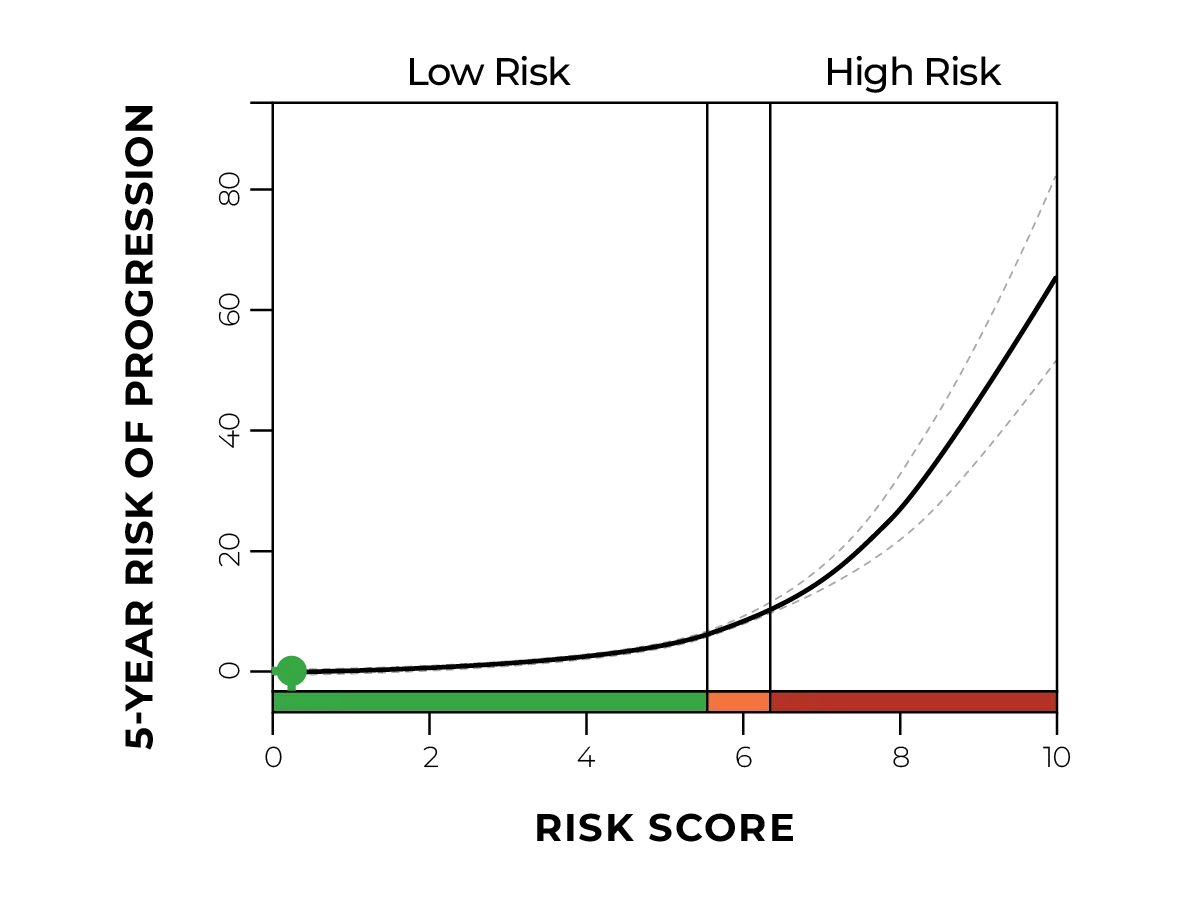
Helena in’t Veld, FNP-C, helped a patient who was skeptical of his risk factors and pathology diagnosis. She leveraged a high-risk TissueCypher score to persuade him to act on his elevated risk of progressing from Barrett’s esophagus (BE) to cancer.
“Having that TissueCypher report, and having the percentage in front of the patient, makes it a lot more real to them. It upstaged our management, and he got endoscopic eradication therapy instead of just being monitored on medication a year later.”
Case details

- 10-year history of acid reflux
- Self-medicated with over-the-counter options
- Higher-than-average alcohol use
- Non-smoker
- BMI 35

- Already scheduled for routine screening colonoscopy
- Textbook case of a patient that should be screened for BE

















.jpg)